Abstract
Introduction. Multicentric Castleman Disease (MCD) is an inflammatory disorder characterized by lymphadenopathy. The clinical course of MCD is variable; some patients have mild symptoms while others develop hypercytokinemia progressing to organ failure. Severely ill patients often have the TAFRO-variety of MCD characterized by Thrombocytopenia, Anasarca, Fever, Reticulin marrow fibrosis, and Organomegaly. We report on 76 MCD patients: the largest series from a single institution.
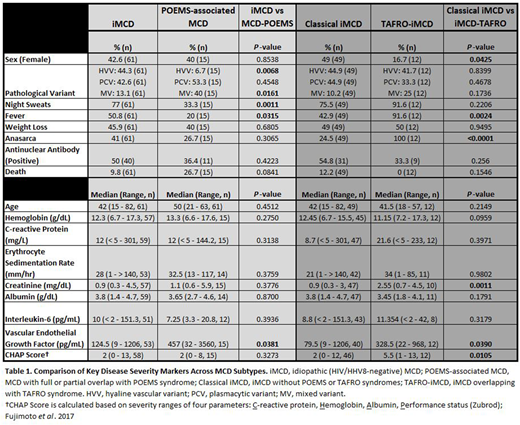
Methods. Data was collected from our institution and outside records via systematic chart review and standardized survey for self-reported symptoms. Laboratory data represent each patient's most severe episode. TAFRO- and non-TAFRO or "classical" iMCD subtypes were grouped (iMCD) for some analyses. Patients were classified as POEMS-associated MCD when they had MCD with full POEMS syndrome or clear features of POEMS.
Results. Forty-nine patients had classical iMCD and 12 TAFRO-iMCD. Fifteen patients had POEMS-associated MCD, of which 8 had coexistent POEMS syndrome. iMCD and POEMS-associated MCD had similar age and sex, but the hyaline vascular variant was more common in iMCD (44.3 vs 6.7%, p=0.006) (Table 1). iMCD patients were more symptomatic in terms of night sweats (61.0 vs 33.3%, p=0.001) and fever (50.8 vs 20%, p=0.031) compared to POEMS-associated MCD, but had similar laboratory characteristics and disease activity (CHAP) scores. TAFRO-iMCD patients were mostly male and had more fever (91.6 vs 42.9%, p=0.002), anasarca (100 vs 24.5%, p<0.0001), higher creatinine (2.6 vs 0.9 mg/dL, p=0.001), poorer CHAP scores (5.5 vs 2.0, p=0.01), and a trend to lower hemoglobin. Interleukin-6 (IL6) levels were not different among groups, but vascular endothelial growth factor (VEGF) was higher in TAFRO-iMCD (328.5 vs 79.5 pg/mL, p=0.034), accounting for anasarca.
Commonly-used treatment regimens for iMCD were the anti-IL6/IL6 receptor antibodies siltuximab and tocilizumab (n=41), rituximab ± steroids (n=23), steroids alone (n=13), and chemotherapy (n=7). There was a high rate of response to anti-IL6 therapy (97%) with a treatment failure (TF) rate of 5%. Two further relapses occurred in patients who discontinued therapy. Steroid monotherapy or rituximab + steroids yielded response rates of 46 and 82%, but were marred by high TF rates (85 and 43%). Chemotherapy responses were noted in 7 instances, but TF occurred twice. There were no significant differences in response to therapy comparing the classical and TAFRO-iMCD groups, but both patients failing anti-IL6 therapy had TAFRO-iMCD. Six TAFRO-iMCD patients received chemotherapy and 2 relapsed. Six patients with POEMS and CD underwent autologous stem cell transplant with major improvement in polyneuropathy and MCD; 2 experienced relapse of their MCD and one died of late myelodysplastic syndrome. One improved post irradiation of a plasmacytoma and 1 died of progressive disease. Most MCD patients with POEMS features received rituximab-based therapies; 6/7 were alive and 1 died of sepsis. There was no difference in overall survival (OS) among the three groups (p=0.35) with a median OS of 5.65 years (4 - 9.2, 95% CI) in the iMCD group, 7.9 years (4.5 - 11.8, 95% CI) in POEMS-associated MCD, and 5.85 years (3.2 - 8.7, 95% CI) in the TAFRO group. The 5-year OS was 91%, 94% and 100% for the iMCD, POEMS-associated MCD and TAFRO groups, respectively.
Conclusions. In a tertiary referral setting, excellent outcomes were achieved in all subgroups, likely attributed to highly selective therapeutic choices. Anti-IL6 therapy for iMCD was reserved for patients with active disease and laboratory evidence of inflammatory syndrome. Some TAFRO-iMCD patients achieved complete responses with anti-IL6 therapy, while others fared well with chemotherapy. Rituximab-based therapy was given to those with more indolent iMCD and those with POEMS-associated MCD. The polyneuropathy of POEMS benefitted most from transplant. Significant differences were noted in VEGF levels both in POEMS-associated MCD and TAFRO-iMCD compared to classical iMCD cases, with each cohort presenting a distinct clinical picture suggesting differing underlying etiologies and cytokine profiles. IL6 levels were not different among groups, though this may be confounded by effects of prior therapy. A better understanding of the pathobiology of the MCD continuum is essential to developing more targeted therapies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal